“The right collagen membrane improves outcome”
Interview with Drs. R Gilbert Triplett and Jay P Malmquist conducted by Todd Scantlebury
Drs. Gilbert Triplett and Jay P Malmquist published the Collagen White Paper in 2020. Up to now, over 8000 copies of the paper have been downloaded or distributed by Osteo Science Foundation.
Drs Triplett and Malmquist, why did you write the Collagen White Paper?
Dr. Malmquist: I felt clinicians need an objective source for understanding collagens and collagen containing biomaterials as both commercial products and building blocks in regenerative procedures. As I recall the genesis of Guided Bone Regeneration and the continuous discussions about barriers versus membranes, collagen has always been in the limelight regarding the so-called “barrier of choice.” Collagen’s impact on implant dentistry and the basic lack of understanding clinicians have for collagen as an adjunct to healing, I thought it was important to define collagen products further.
Dr. Triplett: Collagen is one of the most used biomaterials in dentistry and medicine, yet most practitioners know little about collagen products, and there’s scant scientific evidence for efficacy. Biomaterial companies have been reluctant to conduct comparative trials, so in many cases efficacy is based on anecdotal reports. One example: some collagen companies have not established how long their membranes function or even when they are resorbed. Busy practitioners may not assess their outcomes critically. Therefore, I was interested in participating in this white paper both for my own knowledge and also for our profession.
Why collagen?
Dr. Malmquist: A good question. For me it’s because it’s been the “go-to product” for barrier use in grafting. One has only to review the many product inserts, advertising and misstatements to understand the general lack of understanding that exists. So, when you hear someone say, “all collagens are the same,” that’s why we wrote the paper – to show there are differences. Some clinicians buy on price, but few understand how collagens affect the healing process or the real “cost” of their outcomes. Many clinicians are unaware of the different types of collagens or how they fit into the pathway of regeneration. We hope this paper will help.
Dr. Triplett: Collagens are commonly utilized and have the potential to act as carriers for proteins, growth factors and live cells for tissue regeneration. Yet most clinicians do not know how or why to use one product versus another. Many times scientific evidence is lacking.

What do you think the key, take-home message of the paper is?
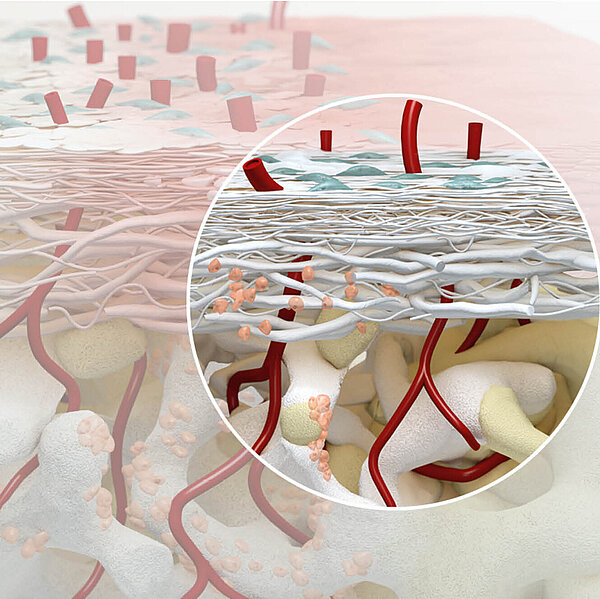
Dr. Malmquist: That collagen is complex in nature, an adjunct to healing and variable in behavior. Certainly, the most important aspect is that collagens are not all the same, and they do not behave the same. Sourcing, cross-linking and processing are key elements in collagen’s behavior.
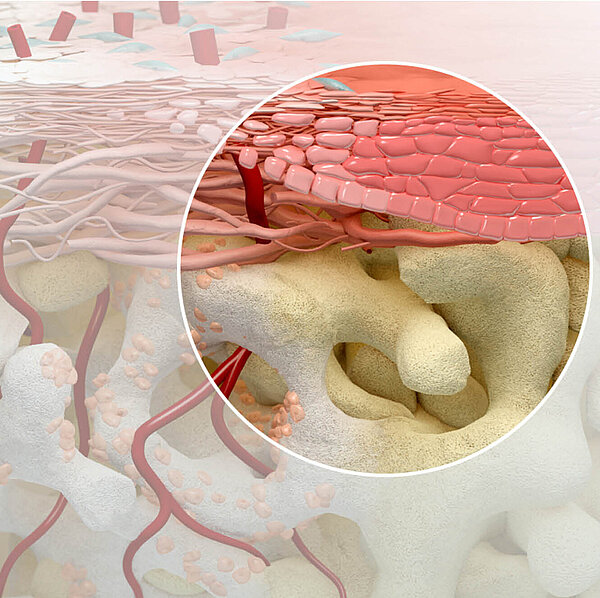
Dr. Triplett: There is utility for the right collagens in hemostasis, clot stabilization, rapid angiogenesis/ vascularization and healing of soft and hard tissues. The right collagens and surgical techniques can provide improved outcomes without complications or morbidity, while also being cost effective and providing better patient care.
You urge manufacturers to “… understand and provide evidence regarding how their collagens interact with healing tissues, especially if their collagen biomaterials are capable of providing regenerative results.” Why, and what makes regenerative results so special?
Dr. Malmquist: Regeneration is critical to improved outcomes. So, the question of whether collagen provides a suitable regeneration platform is critical. Most collagen indications suggest it be used as an adjunct to healing under FDA protocols, and yet we see suggestions of further (off label) uses by the manufactures with little to no evidence. To my way of thinking, this is simply wrong. Unfortunately, this misdirection occurs not only with collagen but with many of the various bone grafting substitutes. There must be adequate science available to substantiate claims.
What’s your advice to young clinicians trying to sort through the variety of biomaterials available today?
Dr. Malmquist: Always depend on the basis of science for determining the best outcome for your patients. This means using products and techniques that are science based and that provide reproducible results. Stay away from gimmicks and unsound science. Understand how products fit into your patient’s healing process. Stay away from products that have no evidence, no real basis for use. For instance, does freeze dried allogeneic bone contain BMP? Probably not, and yet you see this advertised over and over in company literature. Be aware of false or misleading information, look for evidence, listen to the experts that use the products correctly, and make sure they have no conflicts of interest... Is this person being paid for his or her endorsement? This is a very egregious world right now. So, the bottom-line answer is: use products that are steeped in science and evidence.
What is the future for collagen biomaterials and how will this affect the coming generation of surgeons and their patients?
Dr. Malmquist: The future for collagen biomaterials is endless. 3-D constructs will be commonplace, they will be formed with 3-D printing, and they will be embedded with various antibiotics, growth factors and bone proteins. They will also be used as cell carriers, with their bioactive surfaces recruiting cells for faster and better healing. The future is immense or all of us. The interplay of science, regeneration and the improvement of outcomes will influence not only products but lives for years to come. Collagen will be the backbone of many of these projects. To understand collagen is to understand the future of regeneration in medicine and dentistry.
Dr. Triplett: Besides the current use as barrier membranes, hemostatics, etc., the use of collagen in tissue engineering for regeneration of tissue will be a game changer. Collagen scaffolds have been demonstrated to have an effect on the cellular activity within and adjacent to tissue constructs, thus serving as an active rather than passive agent and providing biological interactions and better performance in biological systems.
Will there be more Osteo Science publications like the Collagen White Paper?
Dr. Malmquist: Yes, there will .... our thinking at the Foundation is that we should also write papers concerning growth factors, blood modifiers and associated products to help further define this area of regeneration. The only limiting factor is time. We certainly have the reservoir of talent to do this.
Dr. Triplett: Absolutely. This is only the beginning.
You can download the Collagen White Paper at: www.osteoscience.org/advances