“Soft tissues need to be analyzed as thoroughly as the bone”
The Sequential Ridge Augmentation Protocol helps achieve bone and soft tissue regeneration in the context of implant placement in a systematic way. We discussed with Dr. Neel Bhatavadekar the importance of soft tissues for implant success.
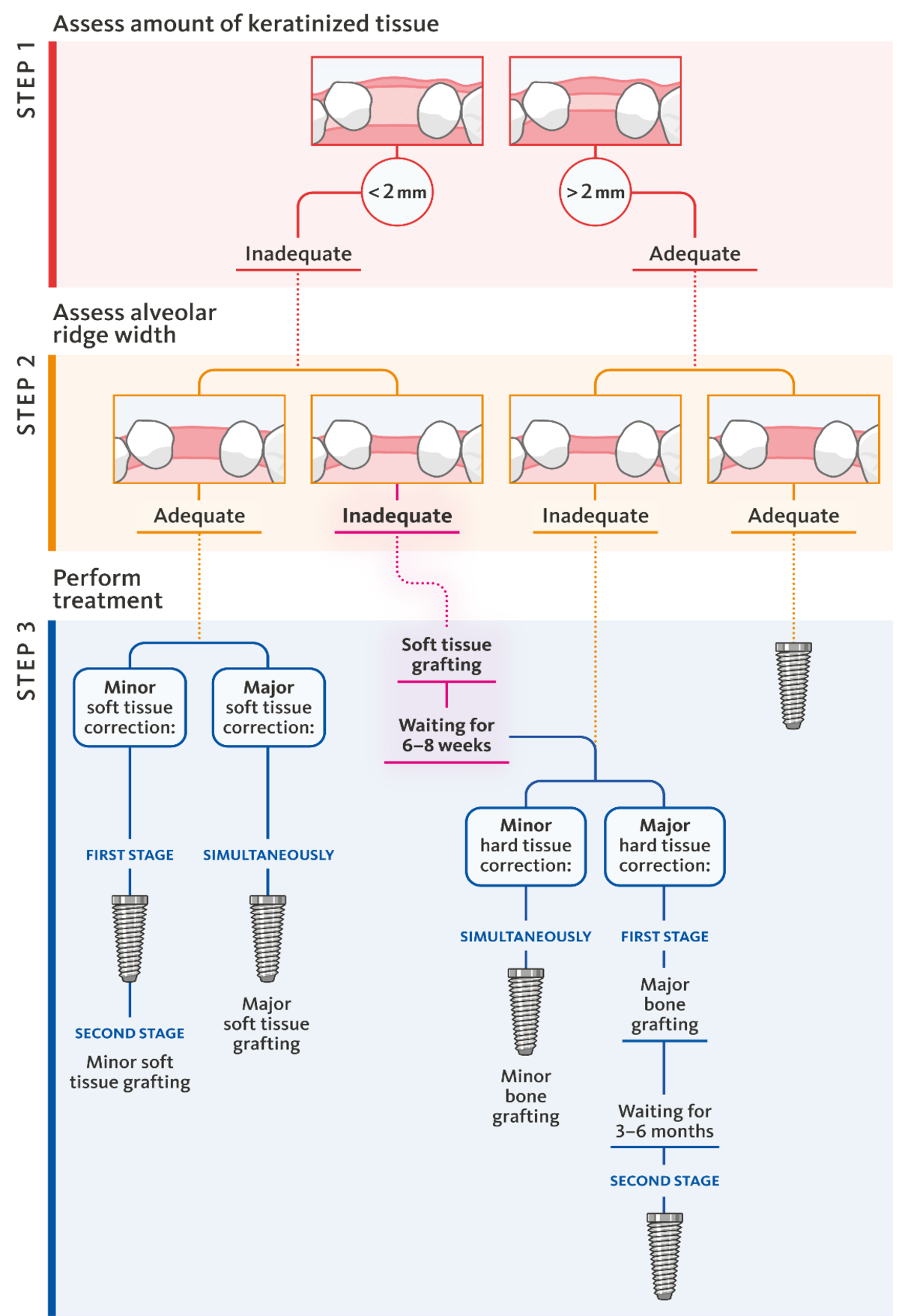
Dr. Bhatavadekar, you have published an algorithm for hard- and soft tissue augmentation in the context of dental implant placement. Step 1 is the assessment of the amount of keratinized tissue. Why is this step 1?
Dr. Bhatavadekar:The soft tissues play an important role for the success of implant therapy.2 We should analyze their status as thoroughly as the state of the bone. This includes assessing the soft tissue thickness and the width of keratinized mucosa. This assessment also tells us how difficult the management of soft tissue may become, if the bone augmentation is extensive.
And there is another reason for assess the keratinized tissue width right from the start. If the patient is not informed about the need to augment soft tissue from the beginning, they consider it less important and sometimes avoid doing it altogether.
Is the importance of keratinized tissue underestimated?
Yes, I feel there is a bias towards bone deficiency.
What are the negative effects of insufficient keratinized tissue around dental implants?
In my experience, in a lot of implant cases with bone augmentation the soft tissue is only considered as an afterthought. This can have negative effects. With an insufficient amount of keratinized tissue, plaque may lead to breakdown of the peri-implant soft tissue.2,3
The debate about whether keratinized tissue improves long-term success is ongoing. Do you see evidence in favor of widening the band of keratinized tissue?
Recent evidence, such as the Osteology Foundation Consensus Report4 confirms the clinical benefits of soft tissue augmentation, by increasing the band of keratinized tissue and soft tissue thickness. Also, in my experience, patients with thicker soft tissue and wider keratinized band—either native or after augmentation—seem to do better long term in that region.
What is the percentage of patients who need soft tissue augmentation in your practice?
In my own practice, about 70% of patients need both hard and soft tissue augmentation together with implant treatment. 30% need only soft tissue augmentation.
Clinicians who attended our courses always tell us that the number of bone and soft tissue procedures in their practices after training is increased. The cases in need of soft tissue augmentation have been always there but they were not recognized as such. “The eye cannot see what the brain does not know.”
Demographic data shows that South Asians have a thin tissue phenotype. Hence, we typically have a greater need for tissue augmentation.
When is the ideal time for creating a wider band of keratinized tissue?
It depends on the width of keratinized tissue at baseline. If there is about 2 mm, one can complete the GBR/implant placement first, and do soft tissue augmentation later. Creating a wider band of keratinized tissue sometimes leads to scar tissue, which is difficult for flap handling during GBR.
But, there are also sites with a very small band of keratinized tissue. This makes the flap closure during GBR both difficult and risky, because of the possibility of mucosal tearing. In these situations, it is better to do the soft tissue augmentation before GBR.
When do you prefer to split bone and soft tissue grafting?
As far as possible, I try to segregate procedures, especially in compromised individuals such as diabetic patients, even if well controlled, mild smokers, etc.
Which techniques and materials do you use?
I have traditionally used the open split thickness flap procedure. But lately, I have also used tunneling. In a recent study from our group5, we found no statistically significant difference between both techniques in root coverage. For anterior esthetic zones, the Vista technique may minimize scar tissue formation.
Regarding material, I have used autogenous tissue extensively, but also allogenic and xenogeneic substitute materials. In India, Geistlich has only recently launched the collagen matrices Geistlich Mucograft® and Geistlich Fibro-Gide®. I have started using these materials, and they offer very promising clinical results, and the possibility of avoiding the palate entirely.
And for bone augmentation?
The materials I use for GBR include Geistlich Bio-Oss® combined with autogenous bone and sometimes allografts. I personally love the handling characteristic of Geistlich Bio-Gide®, since it drapes so well over most grafts.
Since when are you working with this treatment algorithm and has it improved your daily clinical practice?
I have been using this treatment algorithm since 2017, so about 1.5 years before the Sequential Ridge Augmentation protocol was published.
Using the protocol has helped me and my students to easily distinguish which cases need a more staged approach, and to identify surgical cases with a higher risk. It also helps to better prepare the patient for a staged approach from a hard and soft tissue perspective.
References
1. Bhatavadekar NB, Gharpure AS: J Oral Implantol 2018; 44(2): 153-60.
2. Thoma DS, et al.: Clin Oral Implants Res 2018; 29 Suppl 15: 32-49.
3. Lin GH et al.: J Periodontol 2013; 84(12): 1755-67.
4. Giannobile WV, et al.: Clin Oral Implants Res 2018 Mar;29 Suppl 15: 7-10.
5. Bhatavadek.ar NB et al.: Int J Periodontics Restorative Dent 2019; 39(5): 623-30