
Saving teeth affected by periapical defects
Instead of replacing teeth with dental implants, endodontists prefer to prolong the functionality of teeth with traumatized roots. Today advances in procedures and biomaterials allow endodontists to save teeth at an outstanding rate of success.
For saving teeth, clinical success depends heavily on the effectiveness of both periodontal and endodontic treatments.1 In fact, teeth lost during periodontal treatment and so-called “hopeless teeth” are often associated with endodontic problems.
In non-surgical, endodontic treatments, clinicians carefully remove the decay, inflamed or infected pulp, clean, disinfect and shape the root canals, and place a filling to seal the canal. The success rate of this treatment is lower with extensive periapical lesions. In such cases, surgical endodontic treatment is an alternative.
Periapical lesions rank among the most common pathological lesions in alveolar bone.2 Such lesions result in bone defects, and when defects are large, the body fails to regenerate new bone to fill them, and connective tissue may invade the bone defect and impair clinical outcomes.3
Grafting a bone substitute into a defect and covering it with a resorbable membrane can help the body correct the defect. In regenerative endodontic treatments for large defects, as with regenerative periodontal therapy, clinicians use autogenous bone and biomaterials, if not a mixture of both.
Endodontists should diagnose the clinical situation, including access to the canal, location and anatomy of the teeth and surrounding tissues, and in the case of recurrence, the quality of the most recent endodontic treatment. Only then can a proper non-surgical or surgical treatment be performed.
Regenerative periapical microsurgery
Regenerative periapical microsurgery employs fundamental principles of endodontics, periodontics and oral and restorative dentistry. The treatment generally aims at eliminating all factors that could cause periapical lesions, repairing the architecture of lost periapical tissue and preserving the structure and anatomy of the root and soft tissues. It is also important to prevent the recurrence of disease in long-term.
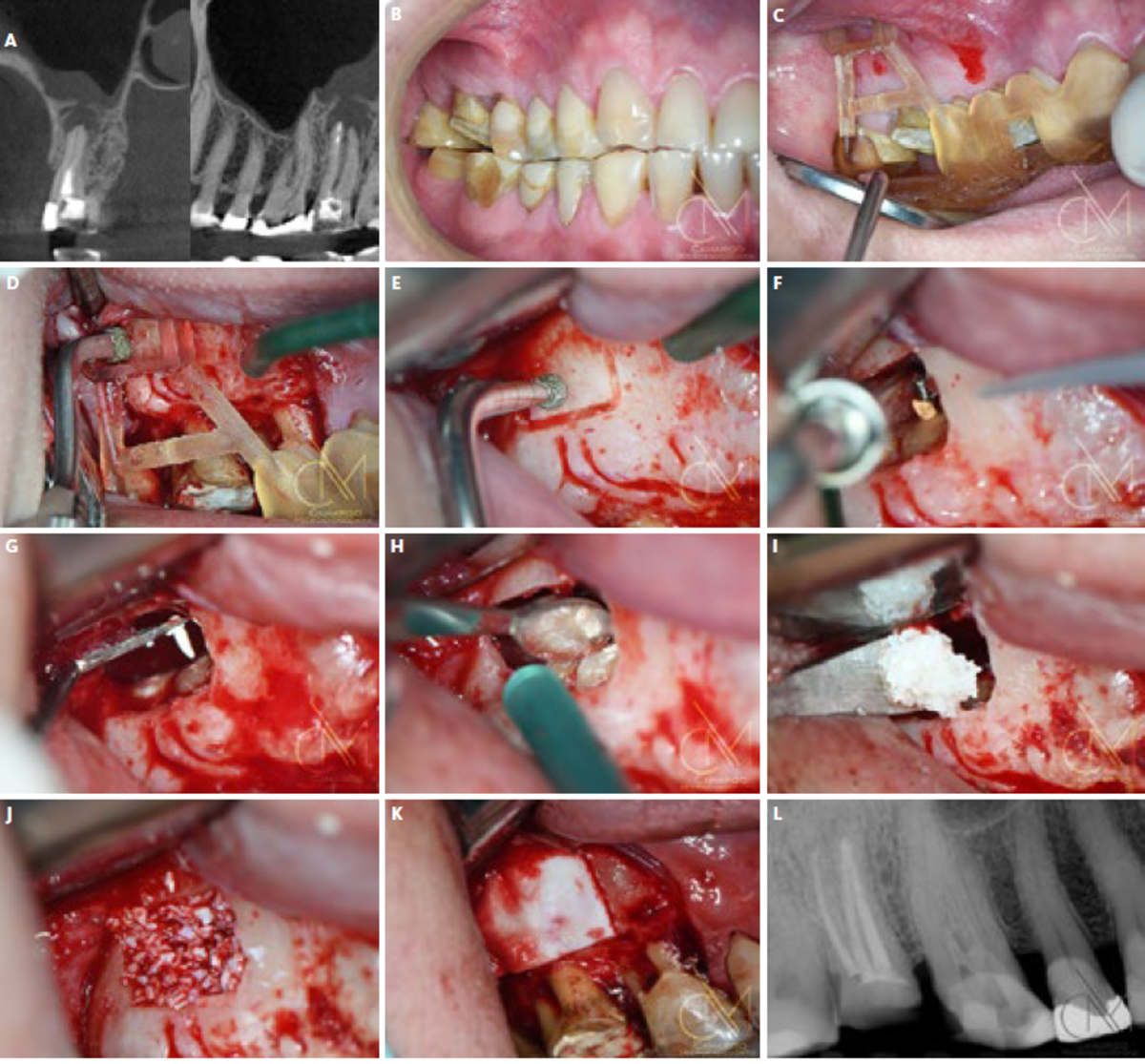
Regenerative periapical microsurgery includes the following steps (Figure 1).
- Enhanced magnification for minimal root resection;
- Ultrasonic root apex preparation;
- Retrograde obturation with a bio-ceramic root repair material; and
- Guided Tissue Regeneration at the site of the bone defect.
Regenerative periapical microsurgery success rates have increased significantly in recent years, thanks to advances in digital planning techniques, microscopy and microsurgical instruments, and biomaterials for Guided Tissue Regeneration.3-4
The choice of regenerative materials
Although autogenous grafts are often considered the gold standard for regenerative dentistry, they are not always the best option. Due to the harvesting procedure, autogenous grafts are associated with greater pain and morbidity. In a systematic review Chavda and Levin (2018) found patients preferred non-autogenous bone graft substitutes, which require fewer days of hospitalization, involve less pain and shorten recovery time.5 The authors found no difference in implant success rate when the alveolar ridge was augmented using different bone grafts, including autogenous bone.5
I use substitute biomaterials for periapical microsurgeries and have been pleased with the clinical outcomes to date. The protocol has allowed me to help many patients preserve their hopeless, natural teeth and keep them healthy and functioning. Recently my colleagues and I published a clinical case report detailing the protocol and clinical outcome for managing a large radicular lesion with regenerative periapical microsurgery.3
The cyst was 40 mm in its largest dimension and involved several anterior teeth, both cortical plates and an extension into the nasal floor. Due to the large size of the defect, we decided to use a mixture of Geistlich Bio-Oss® and autogenous bone from the mandibular ramus, along with platelet-rich fibrin. The clinical outcome was successful 4-years post-surgery (i.e., time of publication). Moreover, when we investigated the cone-beam computed tomography images, we observed well-integrated tissues, new cortical bone and similar radiopacity and trabecular form compared with adjacent, native bone.
To date there are few studies focused on using biomaterials in periapical surgery. Thus, in seeking scientific evidence to explain bone regeneration inside periapical
lesions, we rely primarily on studies conducted in other areas of regenerative therapy. Given the importance of using biomaterials with documented and high-level evidence of long-term benefits compared with other graft materials, Geistlich biomaterials are the gold standard. 7-10
References
- Bröseler F, et al.: J Clin Periodontol. 2017; 44(5):520-9. (clinical study)
- Peters E, Lau M.: J Can Dent Assoc. 2003; 69(9):598–600. (review)
- Camargo JMP, et al.: Oral Surgery. 2019; 12, 323-331. (clinical study)
- Floratos S and Kim S.: Dent Clin North Am. 2017; 61(1):81-91. (review)
- Chavda S and Levin L.: J Oral Implantol. 2018; 44(1):74-84. (review)
- Dietrich T, et al.: Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;95(4):474-82. (clinical study)
- Schwartz Z, et al.: J Periodontol. 2000; 71(8):1258-69. (Pre-clinical study)
- Schneider, O. D. et al.: Acta Biomater. 2009; 5(5):1775-84. (Pre-clinical study)
- Figueiredo M, et al.: J Biomed Mater Res B Appl Biomater. 2010; 92(2):409-19. (Pre-clinical study)
- Lee JS, et al.: Clin Implant Dent Relat Res. 2017; 19(1):140-50. (review)






