
“Orthodontic treatment can start shortly after regenerative surgery.”
We discussed two publications documenting treatment of stage IV periodontitis. Both studies were about the combination of regenerative periodontal surgery and orthodontic tooth movement. Is this a valuable combination? Whom does it help?
Dr. Tietmann, we are talking about patients with stage IV periodontitis. What characterizes them?
Dr. Tietmann: These patients show severe attachment loss and vertical bone loss. The most visible sign of stage IV periodontitis is pathological tooth migration, the typical drifting and flaring of the anterior teeth. You can usually see these patients hiding their smile because they are unhappy about the compromised esthetics. Furthermore, they suffer from functional problems due to the loss of teeth in the posterior region and tooth mobility.
When they come to your office, what is their expectation?
Major concern is to keep their own dentition. Due to the esthetic and functional changes they want to get the migrated teeth realigned and regain esthetics and masticatory function. Very often, pathologic tooth migration of an anterior tooth is the first sign for the patients which makes them seek periodontal treatment. A lot of the patients already had many dental visits and were told their teeth would have to be extracted and would need either implants or removable prostheses.
Implant placement in a patient with a history of severe periodontitis is also not very predictable…
That’s true. Periodontal problems must be solved first, before implants can be placed, and still there is a threat of peri-implantitis, because a history of periodontitis is a risk factor for implants. Within the days of peri-implantitis it is the major goal to keep the natural dentition as long as possible.
How do you usually treat such patients?
It’s a three-step approach. The first step is always to control the infection – anti-infective treatment must be finished before moving on. Second step is periodontal regenerative surgery. This means that I open a flap with minimally invasive surgical techniques to clean the defect and the root and use biomaterials to regenerate the vertical bony defect. It is crucial to stabilize the blood clot during the healing period of regenerative therapy for successful results in mobile teeth. This can be done either by retainers or by implementing the orthodontic appliance before periodontal regenerative surgery starts. And then, the final step is orthodontic treatment. In our retrospective study we started orthodontic tooth movements 3 months postoperatively. Orthodontic counselling has to take place early in the treatment – during anti-infective therapy and before moving on to regenerative therapy. You need to develop a joint vision about the interdisciplinary treatment plan - communication between periodontist und orthodontist is very important in these complex cases.
You published a retrospective study including 48 patients who received periodontal regenerative surgery plus orthodontic treatment, and you had follow-ups up to 4 years.1 What did you learn?
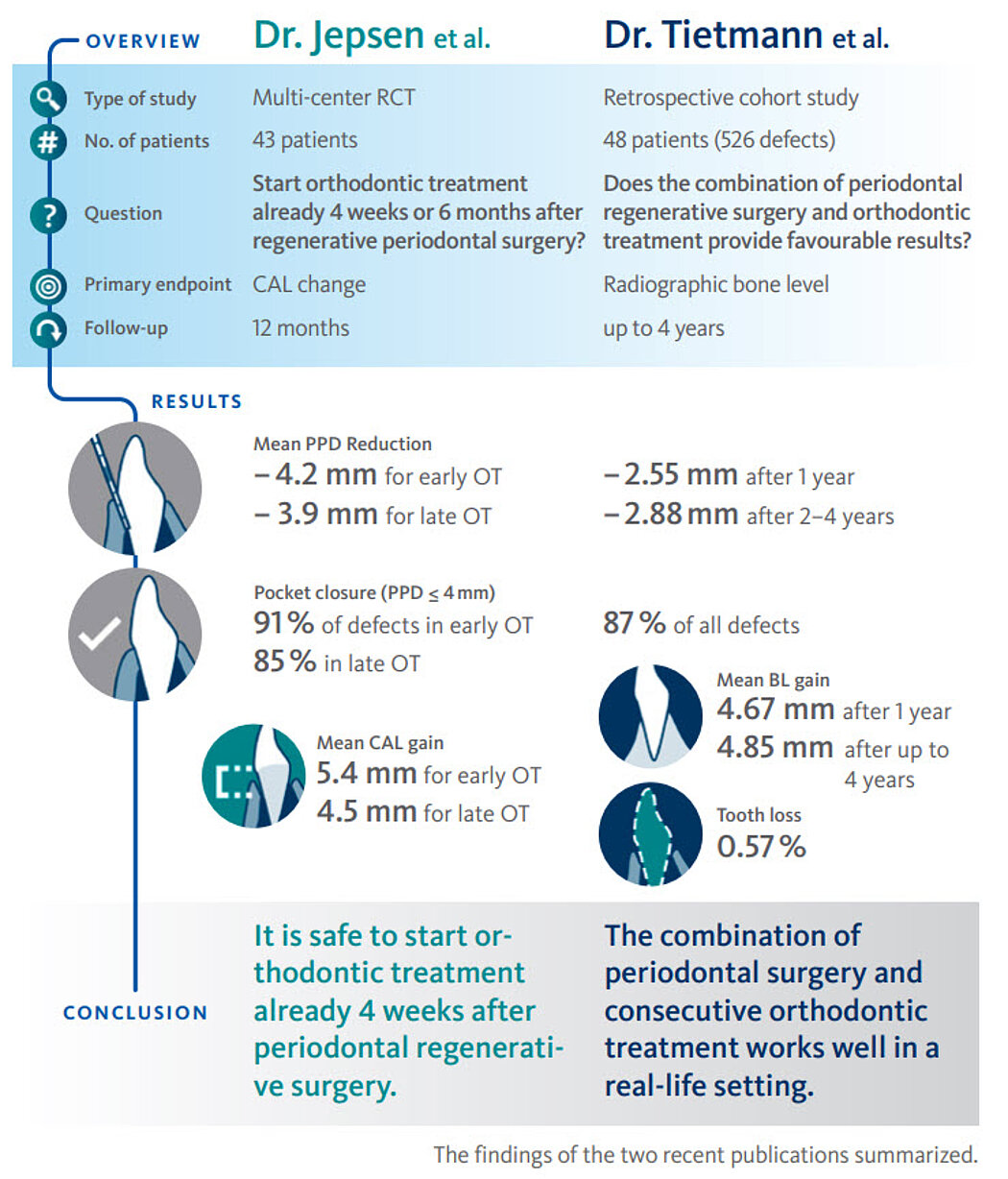
At 1 year we found a mean radiographical bone gain of 4.67mm (see infographic). Also, the pocket reduction was impressive with 87% pocket closure. These findings remained stable or even impoved over time. We only lost 3 out of 526 teeth, not for periodontal but for endodontic reasons. It is important to mention that a majority of these teeth was considered to be “hopeless” at the beginning of the treatment.
What feedback did you get from patients?
Most striking for them was that they could keep their teeth and could smile again. But also regaining function and being able to chew again was very important.
Were they also happy with the cost-benefit ratio of the treatment?
Yes, even if this treatment is expensive I always put the costs into perspective by comparing them with the costs of an implant solution. For such patients, this combined approach is less costly in the long run and more predictable than implant therapy.
Dr. Jepsen, you also investigated this combined approach in a multi-center RCT of 43 patients.2 You focused on the best time point to start the orthodontic treatment. What options are there, and what did you learn?
Dr. Jepsen: We investigated how timing of orthodontic therapy affects outcomes of regenerative periodontal surgery. So far there had not been any prospective randomized controlled clinical trials on this topic. The aim of our study – that was supported by an advanced researcher grant from the Osteology Foundation – was to compare the early initiation of orthodontic therapy (four weeks) and late orthodontic therapy (six months) following regenerative surgery to treat intrabony defects in patients with stage IV periodontitis and pathologic tooth migration and to establish the clinical superiority of one treatment protocol. It was a joint effort of teams from Germany, Italy and Spain.
Did you get a clear result?
Dr. Jepsen: Yes. Clinical attachment gain at 12 months, our primary endpoint, improved in a similar way in both groups. No statistically significant differences between groups could be observed for CAL gain (see infographic). Results with early orthodontic therapy were at least as good as the results achieved after late orthodontic treatment. The outcomes suggest that initiation of orthodontic therapy is possible as early as four weeks after regenerative treatment of intrabony defects, and that significant clinical improvements can be achieved.
Did the result surprise you?
Dr. Jepsen: It was what I had anticipated after having seen the results of previous case series. But guessing is not knowing. Now we know that starting orthodontic treatment early does not impair the healing of the periodontium, provided that the patients perform good oral hygiene and are compliant with supportive care. This will save them a lot of treatment time. Recently, I was invited as an expert to participate in the S3-Level Clinical Practice Guideline Workshop of the European Federation of Periodontology on the treatment of stage IV periodontitis and I was delighted that our findings were well accepted and are now the basis for one of the recommendations.
Could early orthodontic tooth movement even stimulate periodontal wound healing?
Dr. Jepsen: This is possible and it is what we and others assume, but such a conclusion cannot be drawn from a clinical study.
Dr. Tietmann, is this treatment combination of regenerative periodontal surgery and orthodontics recommendable in more cases?
Dr. Tietmann: I think so. We compared the outcome of this combined approach with results from a previous study performed in our private practice when only regenerative periodontal surgery but no orthodontic tooth movement was done.3 Treatment including orthodontic tooth movement delivered around 0.7–0.8mm more radiographic bone gain. The probing pocket depth was reduced even more with the combined therapy. These findings seem to indicate a possible “stimulating” effect of orthodontic tooth movement in the early healing phase on the regenerative outcomes.
You investigated the results over 4 years. What is key for a good, long-term result in such cases?
Dr. Tietmann: Most important is the patients’ compliance. It’s a long therapy – will the patient follow the instructions the entire time? During treatment and afterwards, it is very important to visit regularly with the patient depending on their needs in supportive therapy but at least every 3 months.
On the one hand orthodontic treatment improves the results of periodontal treatment. On the other hand, many case reports show periodontal problems resulting from orthodontic treatment. Do you also experience such cases in your daily practice?
Dr. Jepsen: Oh sure, we are facing very challenging problems. Over-expansion, especially in the lower anterior region, in combination with a thin periodontal phenotype can result in advanced gingival recession. In specific cases retainers in combination with malfunction may lead to very severe recessions on one or two teeth, this is called “wire syndrome.”4 Here we may find incisors with secondary malposition and roots completely outside the bony basis.
Dr. Tietmann: We see this in our dental office as well. And it is not only an esthetic problem. I have had cases with endodontic infections where the apex was nearly exposed.
Dr. Jepsen: So true, and it is very difficult to treat such patients because extraction or placing implants are not an option.
Dr. Jepsen, what are the keys to treating such cases?
Dr. Jepsen: We need to cooperate with orthodontists before recession coverage. Twisted retainers have to be removed, the affected tooth or teeth have to be moved back into their bony housing. Then, after completion of the ortho-treatment these gingival defects can be covered without any complications.
Do orthodontists know about iatrogenic problems after orthodontic treatment?
Dr. Jepsen: More and more orthodontists are aware of this problem. Today we receive many patients referred from orthodontists to evaluate whether their gingiva needs to be augmented before the orthodontic treatment starts. This can be done with grafts and also with soft tissue substitutes. Also, we hope that new EFP-guideline will further improve the close co-operation and communication between orthodontists and periodontists in the future.
References:
- Tietmann C, et al.: J Clin Periodontol 2021; 48:668-678. (clinical study)
- Jepsen K et al.: J Clin Periodontol 2021; 48:1282-92 (clinical study)
- Bröseler F, et al.: J Clin Periodontol 2017; 44:520-9. (clinical study) Illustration: Quiant
- Renkema AM, et al.: Am J Orthod Dentofacial Orthop. 2013; 143(2):206-12. (clinical study)








