"I would fill the gap in any case"
Immediate implant placement is an appealing treatment for patients. Where do you see the biggest advantages?
Prof. Cosyn: The time gain is the biggest advantage. First, from the perspective of the patient, because he or she presents with an urgent problem, and the tooth replacement is performed in one day — the implant and the temporary crown. Second, the practitioner performs only one surgical procedure and one prosthetic procedure. This is really time optimization.
Do you see a global trend towards more and more immediate implant placement?
Prof. Cosyn: Yes, the trend is increasing everywhere. More and more practitioners are performing immediate implant placements, because there is more knowledge about the treatment concept, and clinicians are more aware of the pitfalls. However, this does not mean that the risks of immediate implant placement are fully respected. What worries me most is that the treatment is also expanding into untrained hands.
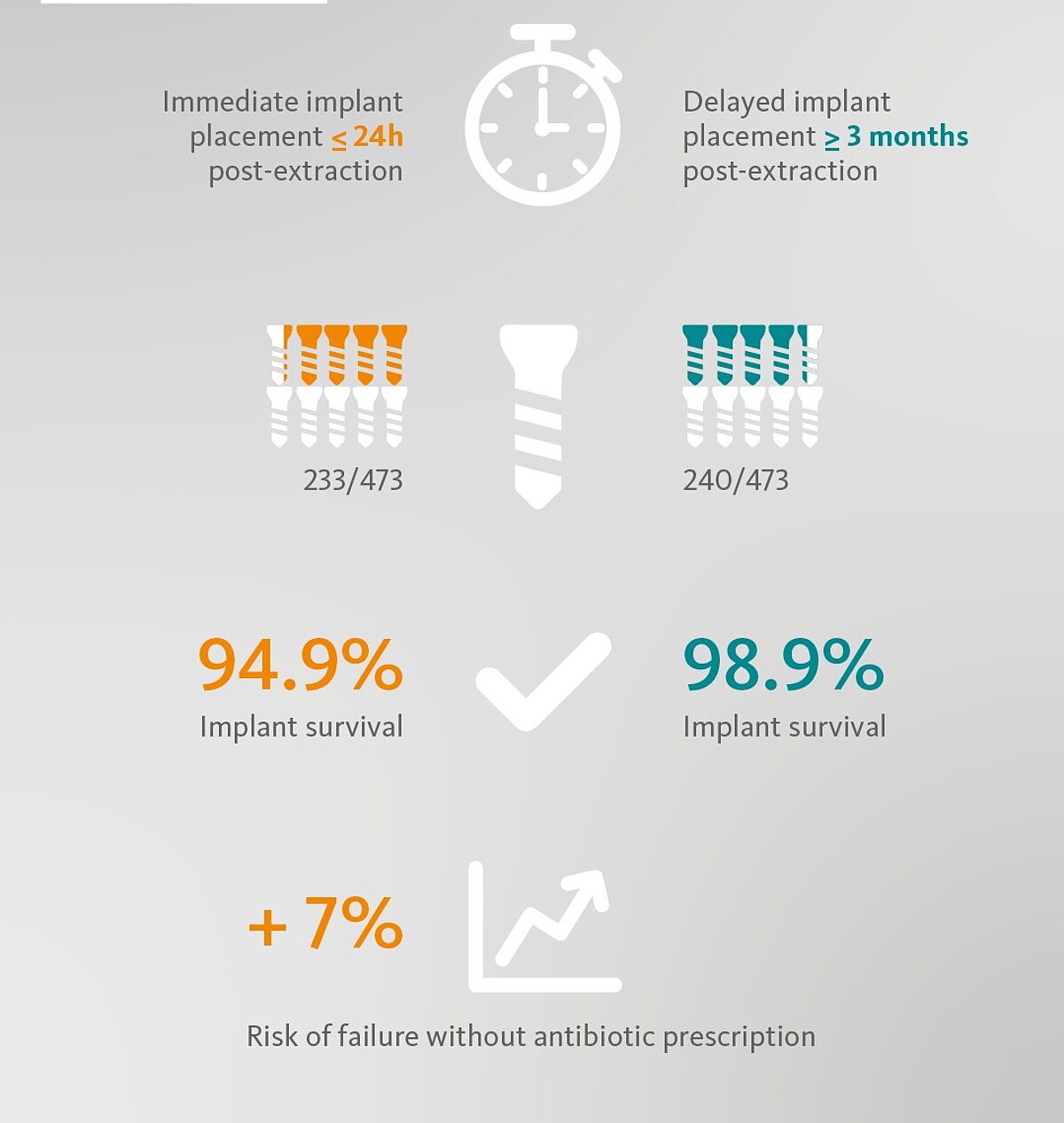
You have recently published a systematic review showing that immediate implant placement has a higher risk for early implant loss than delayed implant placement.1 What are the reasons?
Prof. Cosyn: We did several subgroup analyses on the data, because the entire study was composed of eight diff erent clinical comparative studies. Thanks to the analysis, what has become clear is that the use of post-operative antibiotics has a relevant impact on early implant failure. Not prescribing antibiotics with immediate implants results in a 7% higher risk of failure .
In patients in need of a single implant, will immediate as compared to delayed implnat placement result in different implant survival?
Is it not a general recommendation to prescribe antibiotics after treatment?
Prof. Cosyn: Prescribing antibiotics is not a general recommendation in the context of any implant procedure. This has not been shown, or at least there has been no solid data to confi rm it. The number needed to treat is quite high to have a benefi t in the context of standard implant placement, but this is not the case when you are dealing with immediate implants. It is not possible to generalize for all procedures, but for type I implant placement the use of antibiotics should be considered, and this result is also in accordance with the systematic review of Lang et al. already published in 2012.2
Do you think that hard and soft tissue in the context of immediate implant placement, e.g., “filling the gap”, could make immediate implant placement more predictable?
Prof. Cosyn: I honestly do think so. Ten years ago, there was a debate about the need for socket grafting following immediate implant placement. Now we have three randomized controlled clinical studies,3-5 and the last one by Sanz et al.5 is clearly showing a statistically significant difference in favor of socket grafting versus no grafting. So, for maintaining the integrity of the buccal bone wall, it is imperative to perform grafting. However, we also know that this grafting may not be good enough, as it only reduces buccal bone resorption, it does not eliminate it. Different case series from various research groups show that advanced midfacial recession occurs in about 20% of the cases, which is still too high despite socket grafting and a proper diagnosis. Therefore, the need to compensate opens the indication for soft tissue grafting, in most of the cases.
What are the situations in which you would advise including regenerative treatment as part of the overall treatment?
Prof. Cosyn: In the anterior especially. I think there is no longer a single situation where I would leave out socket grafting. Interestingly, for the first time it has been shown by Sanz et al.5 that the additional effect of socket grafting does not depend on the size of the gap. The proportional effect is the same for either large or small gaps. So, the clinical recommendation is to fill the gap in any case.
And how do you fill the gap?
Prof. Cosyn: I add bovine bone mineral and gently push the biomaterial in an apical direction using a fine plugger. Over-compression should always be avoided.
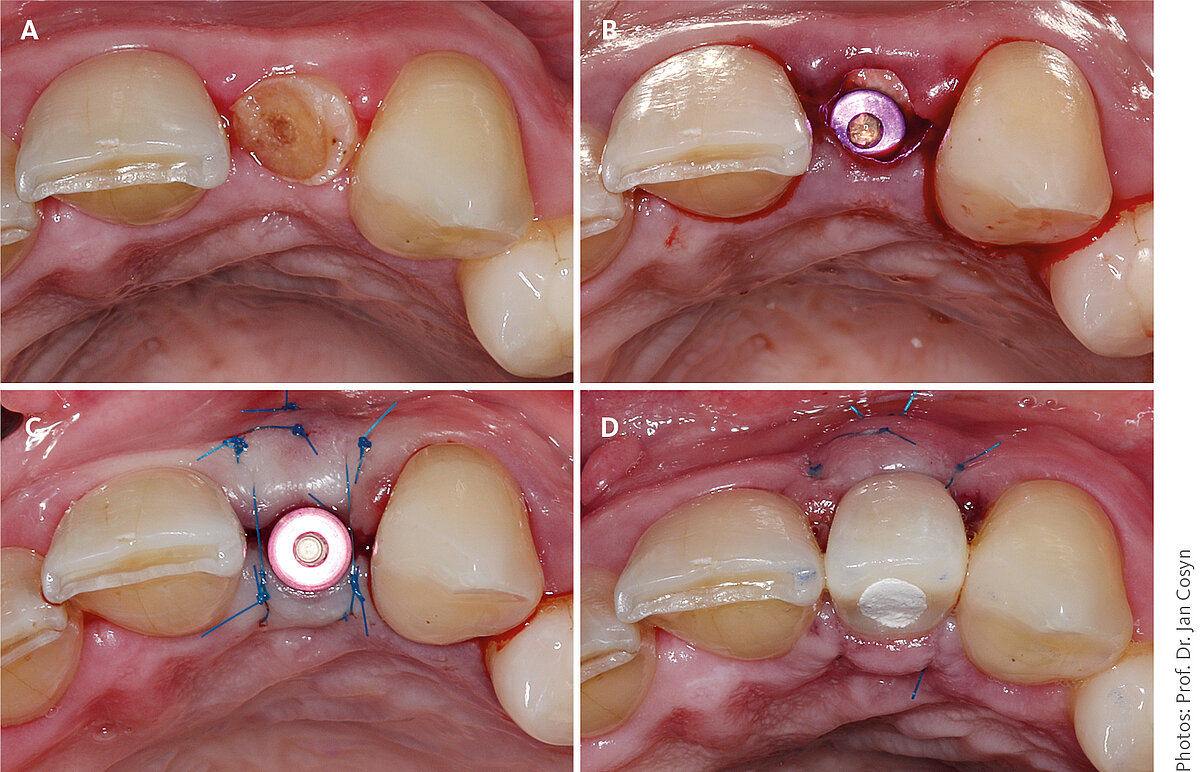
A 58-year-old female patient presented with a broken upper lateral incisor. Because of an intact buccal bone wall and the presence of bone apical and palatal to the extraction socket, type I placement was planned.
When is soft tissue grafting indicated in the context of immediate implant placement?
Prof. Cosyn: I would say frequently. But let's start with the worst scenario – situations where there is no buccal bone. If you have this situation around a tooth, we know that root coverage procedures are predictable, but only if there is at least 1.5 mm of gingival thickness. With an implant case, the thickness must be greater, 2 mm, for the simple reason that there are no inserting supracrestal collagen fibers. There are no data on this, only common sense. Since 2 mm soft tissue thickness is only present in about 10% of the cases, starting with the worst case, this means that, in order to be completely predictable in 90% of cases, soft tissue grafting is necessary.
To fully understand this point: If there is a bone dehiscence, soft tissue augmentation becomes more relevant?
Prof. Cosyn: Soft tissue grafting is nearly always indicated for an optimal and stable outcome. It becomes even more important when there is a bone dehiscence, in my opinion.
What is in your opinion the minimum amount of buccal bone needed to predictably perform immediate implant placement?
Prof. Cosyn: I only perform immediate implant placement when the buccal bone wall is intact. There are some data supporting the concept with small bone dehiscences, but there are no randomized controlled clinical trials or long-term studies on cases lacking more than 50% of the buccal bone wall. Given current knowledge, I don't believe immediate implant placement can be promoted when dealing with compromised buccal bone walls.
Can there be a need for soft tissue thickening even in the presence of intact buccal bone, if the gingival thickness is less than 2 mm?
Prof. Cosyn: I believe there is. In the short term, soft tissue grafting leads to less midfacial recession, as shown in the randomized controlled clinical trial by the Groningen group.6 What I can tell from a 10-year prospective follow-up on single immediate implants in ideal situations in Ghent, is that the soft tissues are more stable when soft tissue grafting was performed. In my view, it is all about longterm tissue stability. Clearly the current knowledge on that is scarce.
Do new techniques, such as 3D imaging, guided surgery or new implant designs, make immediate implant placement more predictable for less experienced surgeons as well?
Prof. Cosyn: They can certainly help. My recommendation is to have a CBCT before tooth extraction or immediate implant placement to make an appropriate diagnosis and to evaluate the risks. It is the only way to visualize the buccal bone wall, its thickness and morphology, and the thickness of the soft tissue, if lip retractors are used. Guided surgery is also important because in type I implant placement, the critical mistake is an implant placed too far buccally. This can happen easily in untrained hands, and no CTG can treat the resulting midfacial recession. So to prevent this possibility, the use of guided surgery is a plus, especially for less experienced surgeons.
Could short and narrow implants circumvent regenerative procedures?
Prof. Cosyn: No, I don’t think so. Short implants are difficult to use in an alveolus, because you need proper bone anchorage. Usually we use longer implants, 11 to 13 mm implants are quite standard for this treatment approach. It’s more important to use small diameters, 3.5 – 3.6 mm, even in the central incisor position, to stay away from the buccal area. And don’t forget, graft the gap in any case.
References
- Cosyn J, et al.: J Clin Periodontol. 2019;46 Suppl 21:224-41 (Systematic review and meta-analysis).
- Lang NP, et al.: Clin Oral Implants Res. 2012;23Suppl 5:39-66 (Clinical study).
- Sanz M, et al.: Clin Oral Implants Res. 2017;28(8):902-10 (Clinical study).
- Chen ST, et al.: Clin Oral Implants Res. 2007;18(5):552-62 (Clinical study).
- Mastrangelo F, et al.: Implant Dent. 2018;27(6):638-45 (Clinical study).
- Zuiderveld EG, et al.: J Periodontol. 2018;89(8):903-14. (Clinical study).